Introduction
The Enhanced Recovery After Surgery protocol represents a multidisciplinary, multimodal approach to perioperative care, designed to attenuate surgical stress and accelerate patient recovery (Modrzyk et al., 2020) (Gramlich et al., 2017). These protocols integrate various evidence-based interventions across the preoperative, intraoperative, and postoperative phases to optimize patient outcomes and reduce complications (Pędziwiatr et al., 2015). Initially applied extensively in major abdominal surgeries, the principles of ERAS protocols have since been adapted and implemented across diverse surgical specialties, including ambulatory settings, demonstrating their broad applicability (Mohamed et al., 2025) (Kaye et al., 2019). The core tenets of ERAS emphasize patient education, rigorous medical optimization, and the minimization of surgical stress responses through standardized care pathways (Huh & Kim, 2021).
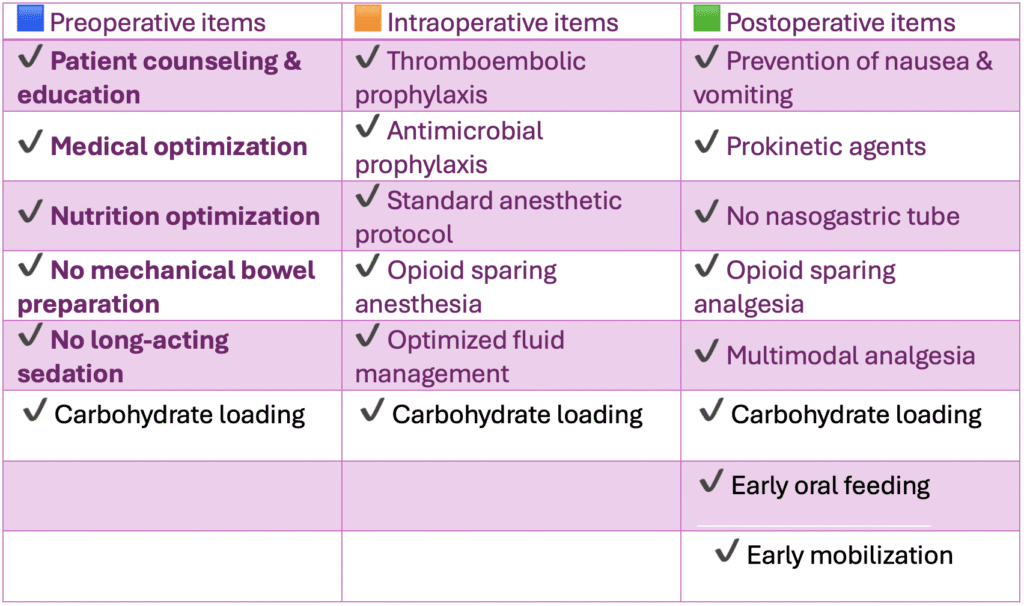
Preoperative Protocolsx of ERAS
Patient Counseling and Education
Effective patient counseling is paramount, ensuring patients comprehend the entire ERAS pathway and actively engage in their recovery process (Gillis et al., 2017). This critical component informs patients about anticipated postoperative experiences, including pain management strategies and early mobilization expectations (Er & ME, 2019). Patient education empowers individuals to become active participants in their recovery, which is crucial for adherence to ERAS guidelines and improved postoperative outcomes (Brodersen et al., 2023). Furthermore, comprehensive preoperative discussions help manage patient expectations, potentially reducing anxiety and enhancing compliance with the protocol (Dr Dinesh ROL 18 Oct.Pdf, n.d.). This includes detailed explanations of the benefits of early ambulation, optimal nutrition, and pain management strategies, thereby fostering a sense of shared responsibility for the recovery process (Soteropulos et al., 2019) (Starkweather & Perry, 2017).
Medical Optimization
Optimal management of comorbidities, such as diabetes and cardiac conditions, prior to surgery is crucial for mitigating perioperative risks and enhancing recovery (Dr Dinesh ROL 18 Oct.Pdf, n.d.). This proactive approach minimizes physiological stressors and prepares the patient’s system for the surgical insult, thereby contributing to a smoother postoperative course and reduced complication rates (Ellis et al., 2021). Such optimization strategies aim to ensure patients are in the best possible physiological state before surgery, which directly contributes to a reduction in hospital stay and improved overall outcomes (Dr Dinesh ROL 18 Oct.Pdf, n.d.).
Thorough preoperative assessment allows for the identification and proactive management of any medical instability, thereby preventing potential intraoperative and postoperative complications (Małczak, 2015). This often involves collaboration between primary care providers, specialists, and the surgical team to achieve specific physiological targets, such as glycemic control or cardiopulmonary stability, prior to the scheduled procedure (Zhang et al., 2022). This comprehensive optimization also involves assessing and addressing factors like anemia and encouraging smoking cessation, further preparing the patient for the demands of surgery and enhancing recovery (Giménez‐Milà et al., 2016).
Nutrition Optimization
Preoperative nutritional status is a critical determinant of surgical outcomes, with malnutrition being a significant risk factor for postoperative complications and prolonged hospital stays. Patients with hypoalbuminemia, for instance, are at a higher risk for surgical-site infections and other adverse events, underscoring the importance of adequate nutritional support and, in some cases, delaying surgery to improve nutritional biomarkers (Evans et al., 2020). Therefore, a comprehensive nutritional assessment and intervention, including dietary counseling and supplementation when necessary, are vital components of the preoperative ERAS protocol (MacMahon et al., 2021). This involves evaluating patients for malnutrition using established tools and initiating appropriate interventions, such as oral nutritional supplements, to improve their nutritional reserves before surgery (Evans et al., 2020).
No Mechanical Bowel Preparation
Historically, mechanical bowel preparation was routinely employed before colorectal surgery; however, current evidence suggests it offers no clear benefit in preventing anastomotic leaks or surgical site infections and may even contribute to dehydration and electrolyte imbalances (Sier et al., 2024). Consequently, its omission in ERAS protocols for various colorectal procedures is now standard practice, streamlining preoperative care (Teeuwen et al., 2009). This eliminates an uncomfortable and potentially harmful step for patients, further enhancing the overall patient experience within the ERAS framework. This approach also avoids the physiological derangements associated with aggressive laxative use, contributing to better fluid and electrolyte balance preoperatively (Taniguchi et al., 2012). The current consensus underscores that mechanical bowel preparation can lead to adverse effects like nausea, vomiting, and electrolyte disturbances, further emphasizing the benefits of its omission (Dr Dinesh ROL 18 Oct.Pdf, n.d.).
No Long-Acting Sedation
The avoidance of long-acting sedatives preoperatively is a key tenet of ERAS, aiming to minimize residual drowsiness and facilitate early postoperative mobilization and cognitive function. This practice ensures a quicker return to baseline mental status, enabling patients to engage more readily in postoperative recovery activities and comply with discharge criteria. The pharmacokinetic properties of short-acting anxiolytics are preferred to minimize postoperative cognitive dysfunction and delirium, especially in elderly populations. This approach also supports earlier ambulation and facilitates adherence to other ERAS components, such as early oral feeding, by reducing potential side effects that could hinder these activities. Instead, short-acting anxiolytics are utilized to alleviate preoperative anxiety without compromising postoperative cognitive function or delaying discharge readiness. This strategic choice in sedation aims to prevent the accumulation of sedative agents, thereby reducing the risk of respiratory depression and delayed recovery (Dr Dinesh ROL 18 Oct.Pdf, n.d.).
Carbohydrate Loading
Preoperative carbohydrate loading involves administering a carbohydrate-rich drink to patients a few hours before surgery, which aims to reduce postoperative insulin resistance and maintain glycogen stores, thereby mitigating the catabolic stress response induced by surgery. This practice has been shown to improve patient comfort, reduce postoperative nausea and vomiting, and accelerate recovery by providing an energy substrate that limits muscle protein breakdown. This intervention also contributes to enhanced patient well-being by reducing the duration of preoperative fasting and alleviating thirst and hunger (Dipasquale et al., 2022) (Roy et al., 2022). This approach contrasts with traditional prolonged fasting protocols, which can exacerbate the stress response and lead to higher rates of postoperative complications. Furthermore, carbohydrate loading has been demonstrated to reduce the incidence of postoperative hyperglycemia and maintain glucose homeostasis, critical for optimal wound healing and immune function.
Intraoperative Protocols of ERAS
Thromboembolic Prophylaxis
Deep vein thrombosis and pulmonary embolism represent significant postoperative complications, making robust thromboembolic prophylaxis a cornerstone of intraoperative ERAS protocols. This typically involves a combination of mechanical and pharmacological methods tailored to individual patient risk profiles to minimize the incidence of these potentially life-threatening events (Trotta et al., 2019). This critical intervention is often initiated preoperatively and continues throughout the intraoperative period, often extending into the postoperative phase to ensure sustained protection. Current guidelines often recommend the use of low molecular weight heparin or unfractionated heparin, alongside intermittent pneumatic compression devices, to actively prevent thrombus formation during and after surgery.
Antimicrobial Prophylaxis
Administering prophylactic antibiotics is crucial for preventing surgical site infections, a common cause of morbidity, and should be carefully timed to ensure adequate tissue concentrations during incision and throughout the procedure (Romero et al., 2020). This prophylactic measure is administered within 60 minutes prior to incision, with re-dosing during prolonged procedures or in cases of significant blood loss, aligning with established guidelines for preventing postoperative infections (Dr Dinesh ROL 18 Oct.Pdf, n.d.). The selection of the appropriate antibiotic agent is guided by the anticipated microbial flora associated with the surgical site, aiming for broad-spectrum coverage against common pathogens without promoting antimicrobial resistance.
This targeted approach minimizes the risk of infection while adhering to principles of antimicrobial stewardship, a critical consideration in modern surgical practice. Moreover, adherence to strict aseptic techniques and environmental controls within the operating room further supplements the effectiveness of antimicrobial prophylaxis in preventing surgical site infections. This comprehensive strategy ensures a multilayered defense against potential pathogenic invasion, contributing significantly to improved patient outcomes and reduced healthcare burdens. (Giménez‐Milà et al., 2016)
Standard Anesthetic Protocol
A standardized anesthetic protocol is essential within ERAS frameworks to ensure consistency, minimize variability, and optimize patient outcomes by employing a balanced approach to general anesthesia (Bloria et al., 2021). This involves careful selection of anesthetic agents and techniques to maintain physiological stability, facilitate rapid emergence, and support early postoperative recovery. The protocol often emphasizes the use of short-acting agents, multimodal analgesia, and regional anesthetic techniques to reduce opioid consumption and expedite recovery from anesthesia (Jakobsson et al., 2017). This methodical approach not only enhances immediate postoperative comfort but also contributes to reduced hospital stays and improved patient satisfaction (Carcéles et al., 2025).
For instance, the use of isoflurane is often preferred over other volatile anesthetics due to its lower arrhythmogenic and myocardial depressive effects (Dr Dinesh ROL 18 Oct.Pdf, n.d.). Such careful selection contributes to stable intraoperative hemodynamics, which is crucial for preventing complications and promoting faster recovery, especially in patients with cardiovascular comorbidities (Dr Dinesh ROL 18 Oct.Pdf, n.d.). The induction of anesthesia itself is a critical period where close monitoring is essential, particularly for preventing post-induction hypotension, which can compromise organ perfusion and lead to adverse outcomes (Aïssaoui et al., 2022). Perioperative management goals typically include maintaining a mean arterial pressure between 70–110 mm Hg and a hemoglobin concentration above 10 g/dL to ensure adequate tissue oxygenation (Jakobsson et al., 2017).
However, it is crucial to recognize that the hemodynamic and ventilatory effects of laparoscopic surgery, particularly abdominal insufflation, may elevate cardiovascular risk, especially in patients with pre-existing conditions like congestive heart failure, ischemic heart disease, or pulmonary hypertension (Dr Dinesh ROL 18 Oct.Pdf, n.d.). Consequently, precise anesthetic management is critical, encompassing careful titration of agents, vigilant hemodynamic monitoring, and prompt intervention to mitigate these risks (Jakobsson et al., 2017).
Opioid Sparing Anesthesia
Therefore, anesthetic techniques should prioritize opioid-sparing strategies, such as regional anesthesia and multimodal analgesia, to reduce perioperative opioid exposure and its associated adverse effects. This approach aims to minimize common opioid-related side effects, including postoperative nausea and vomiting, ileus, respiratory depression, and prolonged hospital stays, thereby enhancing patient recovery and satisfaction (Fu et al., 2025). Regional anesthesia, including neuraxial blocks or peripheral nerve blocks, can significantly reduce systemic opioid requirements while providing superior analgesia (Corte et al., 2022).
Optimized Fluid Management
Optimized fluid management within ERAS protocols focuses on maintaining euvolemia to prevent complications associated with both hypovolemia and fluid overload (Roy et al., 2022). This precise approach involves individualized fluid administration based on physiological parameters and surgical demands, aiming to maintain adequate tissue perfusion without compromising cardiac function or increasing interstitial edema. Goal-directed fluid therapy, often guided by dynamic measures of fluid responsiveness, has emerged as a cornerstone of optimized fluid management, allowing for precise adjustments in intravenous fluid administration (Jakobsson et al., 2017). This approach is particularly critical given that both hypovolemia, which can lead to decreased cerebral blood flow and acute kidney injury, and hypervolemia, which can result in pulmonary edema and delayed recovery, are associated with increased morbidity (Bloria et al., 2021).
Preventing Hypothermia
Preventing perioperative hypothermia is paramount, as it is associated with adverse outcomes such as increased blood loss, surgical site infections, and delayed recovery from anesthesia. Maintenance of normothermia is achieved through active warming techniques, including forced-air warmers, warmed intravenous fluids, and insulated blankets, throughout the perioperative period (Jakobsson et al., 2017). This proactive thermal management strategy not only enhances patient comfort but also contributes to better surgical outcomes by minimizing physiological stress responses. Furthermore, rigorous temperature monitoring ensures that normothermia is consistently maintained, preventing fluctuations that could negatively impact recovery (Jakobsson et al., 2017). The maintenance of core body temperature is a dynamic process, and vigilant monitoring allows for timely adjustments to warming interventions, thereby preventing even mild degrees of hypothermia (Bandyopadhyay et al., 2019).
Postoperative Protocols of ERAS
Prevention of Nausea and Vomiting
Postoperative nausea and vomiting represent a significant source of patient discomfort and can delay discharge, necessitating a prophylactic approach using antiemetic agents based on individual patient risk factors. This proactive management strategy often involves a multimodal approach, combining different classes of antiemetics to target various pathways implicated in emesis, thereby maximizing efficacy (Fu et al., 2025). Pharmacological interventions, such as serotonin antagonists, corticosteroids, and dopamine antagonists, are frequently combined to optimize prevention in high-risk patients. Additionally, mild intraoperative hypercapnia has been shown to reduce the incidence of postoperative nausea and vomiting and shorten emergence and recovery times from general anesthesia (Dr Dinesh ROL 18 Oct.Pdf, n.d.). This approach aims to minimize common opioid-related side effects, including postoperative nausea and vomiting, ileus, respiratory depression, and prolonged hospital stays, thereby enhancing patient recovery and satisfaction (Dr Dinesh ROL 18 Oct.Pdf, n.d.).
Prokinetic Agents
Prokinetic agents are utilized in ERAS protocols to stimulate gastrointestinal motility, thereby mitigating postoperative ileus and facilitating earlier return of bowel function. These agents, such as metoclopramide or erythromycin, promote coordinated contractions of the gastrointestinal tract, accelerating the transit of luminal contents and reducing symptoms like abdominal distension and nausea. This accelerated recovery of bowel function is crucial for early oral feeding and overall patient comfort, contributing significantly to a shorter hospital stay (Dr Dinesh ROL 18 Oct.Pdf, n.d.). Their strategic use within the ERAS framework underscores a comprehensive approach to gastrointestinal recovery, preventing complications associated with prolonged ileus. The judicious application of prokinetic agents, tailored to individual patient needs and surgical context, further exemplifies the personalized medicine approach inherent in ERAS.
No Nasogastric Tube
The routine use of nasogastric tubes for gastric decompression is typically avoided in ERAS protocols due to their association with patient discomfort, increased risk of pulmonary complications, and delayed recovery of gastrointestinal function. Instead, selective placement is reserved for specific indications, such as intractable vomiting or bowel obstruction, to minimize their impact on patient recovery and promote earlier oral intake. This selective approach prevents the disruption of upper gastrointestinal integrity and reduces the potential for sinusitis or otitis media, which can arise from prolonged intubation.
Eliminating routine nasogastric tube insertion is a key component of ERAS, aligning with the overall goal of minimizing invasive interventions and promoting a more physiological recovery. This strategy allows for reduced postoperative ileus and other surgical complications, contributing to a decrease in hospital length of stay and readmission rates (Wells et al., 2021). Furthermore, avoiding routine nasogastric intubation supports earlier mobilization and oral feeding, both integral to accelerated recovery pathways and enhanced patient outcomes (Heathcote et al., 2019).
Opioid Sparing Analgesia
A central tenet of ERAS protocols is the implementation of opioid-sparing analgesia, a multimodal approach that integrates various pharmacological and non-pharmacological methods to achieve effective pain control while minimizing opioid-related side effects. This strategy leverages regional anesthesia, non-steroidal anti-inflammatory drugs, acetaminophen, and gabapentinoids, thereby reducing the reliance on opioids and their associated adverse events such as respiratory depression, constipation, and postoperative nausea and vomiting. This comprehensive approach to pain management not only enhances patient comfort but also facilitates earlier mobilization and a more rapid return to normal activities, contributing to a shorter hospital stay (Huang et al., 2024; Zhou et al., 2021).
Multimodal Analgesia
Multimodal analgesia, an integral component of ERAS protocols, combines several analgesic agents and techniques acting on different pain pathways to achieve superior pain control with reduced individual drug dosages and fewer side effects (Afonso et al., 2019) (Thompson et al., 2018). This strategy is crucial for effective postoperative pain management, significantly improving patient outcomes such as pain levels, functional recovery, and overall satisfaction (Chen et al., 2021). By targeting various nociceptive mechanisms simultaneously, multimodal analgesia minimizes the reliance on a single class of analgesics, particularly opioids, thereby mitigating their dose-dependent adverse effects.
This approach, frequently involving a combination of regional blocks, non-steroidal anti-inflammatory drugs, and acetaminophen, significantly contributes to enhanced recovery by facilitating earlier mobilization and rehabilitation (Othenin‐Girard et al., 2025) (Loria et al., 2022). Effective postoperative pain control without adverse effects of analgesic medications is essential for rapid recovery (Park et al., 2023). Furthermore, optimizing pain management through multimodal analgesia lessens the need for postoperative analgesics and aids in early mobilization, which is critical for preventing complications and improving functional outcomes (Chitnis et al., 2020; Jain et al., 2023).
Oral Nutritional Supplements
Oral nutritional supplements are frequently incorporated into ERAS protocols to support patient recovery by providing essential macronutrients and micronutrients, especially in surgical patients who may have increased metabolic demands or compromised nutritional status. These supplements can bridge nutritional gaps, particularly in the immediate postoperative period when oral intake might be limited, ensuring adequate caloric and protein intake to support wound healing and immune function. They are particularly beneficial for malnourished patients or those undergoing major surgery, as they have been shown to improve clinical outcomes, reduce complications, and decrease hospital length of stay (Chiu et al., 2018). Preoperative nutritional optimization, which often includes oral nutritional supplements, helps build nutritional reserves that are vital for tolerating surgical stress and promoting a robust recovery (Elsayed, 2020). This proactive approach ensures that patients enter surgery in the best possible nutritional state, minimizing postoperative catabolism and accelerating the restorative process (Awad et al., 2019).
Early Oral Feeding
Early oral feeding is a cornerstone of ERAS protocols, challenging traditional practices that advocated for prolonged postoperative fasting due to concerns about anastomotic leaks and ileus. Current evidence strongly supports the safety and efficacy of early oral feeding, demonstrating improved gut motility, reduced infectious complications, and a shorter hospital stay (Canzan et al., 2022) (Fakhar et al., 2021). This approach also enhances patient comfort and satisfaction, aligning with the patient-centered philosophy of ERAS. Initiating oral intake soon after surgery stimulates gastrointestinal function, decreases the incidence of paralytic ileus, and maintains the integrity of the gut mucosa (Wobith & Weimann, 2021).
Moreover, early enteral nutrition prevents gut mucosal atrophy and reduces bacterial translocation, thereby lowering the risk of systemic infections and improving overall postoperative recovery (Evans et al., 2020). This practice is widely supported by research for both upper and lower gastrointestinal surgeries, demonstrating significant reductions in morbidity and hospital length of stay (Hao et al., 2021).
Early Mobilization
Early mobilization is a fundamental component of ERAS protocols, designed to counteract the deleterious physiological effects of prolonged bed rest and accelerate postoperative recovery. This practice encompasses a range of activities, from sitting up in bed and ambulating within hours of surgery to progressive increases in physical activity, significantly reducing the risk of complications such as venous thromboembolism, pulmonary issues, and muscle atrophy (Bandyopadhyay et al., 2019). It also mitigates postoperative cognitive dysfunction and improves functional independence, thereby facilitating a quicker return to baseline activities (Stuart et al., 2024) (Park et al., 2021). Active participation in early mobilization programs, often guided by physical therapists and nurses, is crucial for restoring strength, endurance, and overall functional capacity, ultimately shortening recovery times and enhancing long-term patient outcomes.
This strategy has been consistently shown to decrease hospital length of stay and improve overall recovery trajectories across various surgical specialties (Basse et al., 2000; Deng et al., 2022). Furthermore, early mobilization not only reduces the risk of postoperative complications but also enhances patient morale and satisfaction, reinforcing the holistic approach of ERAS (Seow‐En et al., 2020). Successful implementation of ERAS protocols, incorporating all these evidence-based interventions, has consistently demonstrated improvements in patient outcomes, including reduced complication rates, shorter hospital stays, and enhanced patient satisfaction (Li et al., 2022) (Tweed et al., 2022) (Agnoletti, 2020).
The consistent adherence to these multifaceted ERAS interventions has been directly linked to improved clinical outcomes, including reduced morbidity and mortality, as demonstrated in numerous studies (Pisarska et al., 2018). A novel pilot study, for instance, showed that adopting simple techniques derived from ERAS principles can significantly reduce postoperative morbidities in specific surgical contexts (Bandyopadhyay et al., 2019).
Discussion
The comprehensive integration of these individualized components within a cohesive ERAS framework underpins its efficacy in optimizing patient recovery and streamlining healthcare resource utilization (Arrick et al., 2018). This approach represents a paradigm shift in perioperative care, moving from traditional practices to an evidence-based, patient-centered methodology that standardizes and improves the quality of surgical care (Debas et al., 2025) (Stethen et al., 2018) (Bandyopadhyay et al., 2019). Despite the demonstrated benefits, successful implementation of ERAS protocols continues to face various barriers, including surgeon resistance to change, lack of institutional support, and insufficient education among healthcare providers (Pearsall et al., 2014).
Effective strategies for overcoming these hurdles often involve multidisciplinary team engagement, continuous staff training, and robust auditing mechanisms to ensure compliance and identify areas for improvement (Pache et al., 2021). Moreover, continuous research and adaptation of ERAS guidelines based on emerging evidence are essential to further refine protocols and maximize their impact on patient outcomes (Zhang et al., 2025). For instance, high compliance with ERAS pathway components is directly associated with improved clinical outcomes and reduced healthcare utilization in elective colorectal surgery (Fischer et al., 2021).
This emphasizes the critical need for a concerted effort from all stakeholders to ensure the widespread and consistent adoption of these protocols, thereby translating research findings into tangible patient benefits (Zorrilla‐Vaca et al., 2021). However, challenges such as time restraints, reluctance to change, and logistical complexities can impede the successful integration of ERAS protocols into routine clinical practice (Martín et al., 2017) (Yoon & Lee, 2024).
Conclusion
ERAS protocols, when meticulously implemented, have demonstrated significant improvements in patient recovery and reduced complications across diverse surgical disciplines.
References:
- Afonso, A. M., Tokita, H. K., McCormick, P. J., & Twersky, R. S. (2019). Enhanced Recovery Programs in Outpatient Surgery [Review of Enhanced Recovery Programs in Outpatient Surgery]. Anesthesiology Clinics, 37(2), 225. Elsevier BV. https://doi.org/10.1016/j.anclin.2019.01.007
- Agnoletti, V. (2020). Implementation of an Enhanced Recovery Program after Bariatric Surgery: Clinical and Cost-Effectiveness Analysis. Acta Clinica Croatica. https://doi.org/10.20471/acc.2020.59.02.05
- Aïssaoui, Y., Jozwiak, M., Bahi, M., Belhadj, A., Alaoui, H., Qamous, Y., Serghini, I., & Seddiki, R. (2022). Prediction of post-induction hypotension by point-of-care echocardiography: A prospective observational study. Anaesthesia Critical Care & Pain Medicine, 41(4), 101090. https://doi.org/10.1016/j.accpm.2022.101090
- Arrick, L., Mayson, K., Hong, T., & Warnock, G. L. (2018). Enhanced recovery after surgery in colorectal surgery: Impact of protocol adherence on patient outcomes. Journal of Clinical Anesthesia, 55, 7. https://doi.org/10.1016/j.jclinane.2018.12.034
- Awad, H. M., Ahmed, A., RD, U., Stoicea, N., & SD, B. (2019). Potential role of pharmacogenomics testing in the setting of enhanced recovery pathways after surgery. DOAJ (DOAJ: Directory of Open Access Journals). https://doaj.org/article/76f1610b155644c7a14baabf52f0dcc3
- Bandyopadhyay, A., Talwar, R., Patel, A., & Jaiswal, P. (2019). The modifications in surgical technique and its impact on short term morbidity in modified radical mastectomy: a tertiary care hospital experience. International Surgery Journal, 6(12), 4354. https://doi.org/10.18203/2349-2902.isj20195393
- Basse, L., Jakobsen, D. H., Billesbølle, P., Werner, M. U., & Kehlet, H. (2000). A Clinical Pathway to Accelerate Recovery After Colonic Resection. Annals of Surgery, 232(1), 51. https://doi.org/10.1097/00000658-200007000-00008
- Bloria, S., Panda, N., Jangra, K., Bhagat, H., Mandal, B., Kataria, K., Chauhan, R., Luthra, A., Soni, S. L., Kaloria, N., Mahajan, S., Paul, S. K., Gupta, S., Agrawal, S., & Singla, N. (2021). Goal-directed Fluid Therapy Versus Conventional Fluid Therapy During Craniotomy and Clipping of Cerebral Aneurysm: A Prospective Randomized Controlled Trial. Journal of Neurosurgical Anesthesiology, 34(4), 407. https://doi.org/10.1097/ana.0000000000000769
- Brodersen, F., Wagner, J., Uzunoǧlu, F. G., & Petersen‐Ewert, C. (2023). Impact of Preoperative Patient Education on Postoperative Recovery in Abdominal Surgery: A Systematic Review [Review of Impact of Preoperative Patient Education on Postoperative Recovery in Abdominal Surgery: A Systematic Review]. World Journal of Surgery, 47(4), 937. Springer Science+Business Media. https://doi.org/10.1007/s00268-022-06884-4
- Canzan, F., Caliaro, A., Cavada, M. L., Mezzalira, E., Paiella, S., & Ambrosi, E. (2022). The effect of early oral postoperative feeding on the recovery of intestinal motility after gastrointestinal surgery: Protocol for a systematic review and meta-analysis [Review of The effect of early oral postoperative feeding on the recovery of intestinal motility after gastrointestinal surgery: Protocol for a systematic review and meta-analysis]. PLoS ONE, 17(8). Public Library of Science. https://doi.org/10.1371/journal.pone.0273085
- Carcéles, A. F., Degani, M., Soler, C., Aguado, C. I. S., Fernández, N., Mateo, A. G. de C., Herrería‐Bustillo, V. J., Franco, C. D., & Briganti, A. (2025). Veterinary Enhanced Recovery After Surgery (Vet-ERAS) Program in Dogs Undergoing Emergency Laparotomy. Veterinary Sciences, 12(4), 377. https://doi.org/10.3390/vetsci12040377
- Chen, Q., Chen, E., & Qian, X. (2021). A Narrative Review on Perioperative Pain Management Strategies in Enhanced Recovery Pathways—The Past, Present and Future [Review of A Narrative Review on Perioperative Pain Management Strategies in Enhanced Recovery Pathways—The Past, Present and Future]. Journal of Clinical Medicine, 10(12), 2568. Multidisciplinary Digital Publishing Institute. https://doi.org/10.3390/jcm10122568
- Chitnis, S., Tang, R., & Mariano, E. R. (2020). The role of regional analgesia in personalized postoperative pain management [Review of The role of regional analgesia in personalized postoperative pain management]. Korean Journal of Anesthesiology, 73(5), 363. Korean Society of Anesthesiologists. https://doi.org/10.4097/kja.20323
- Chiu, C., Aleshi, P., Esserman, L. J., Inglis-Arkell, C., Yap, E. N., Whitlock, E. L., & Harbell, M. W. (2018). Improved analgesia and reduced post-operative nausea and vomiting after implementation of an enhanced recovery after surgery (ERAS) pathway for total mastectomy. BMC Anesthesiology, 18(1). https://doi.org/10.1186/s12871-018-0505-9
- Corte, L. D., Mercorio, A., Palumbo, M., Viciglione, F., Cafasso, V., Candice, A., Bifulco, G., & Giampaolino, P. (2022). Minimally invasive anesthesia for laparoscopic hysterectomy: a case series. Archives of Gynecology and Obstetrics, 306(6), 2001. https://doi.org/10.1007/s00404-022-06727-6
- Debas, S. A., Chekol, W. B., Zeleke, M. E., & Mersha, A. T. (2025). Delayed ambulation in adult patients after major abdominal surgery in Northwest Ethiopia: a multicenter prospective follow up study. Scientific Reports, 15(1). https://doi.org/10.1038/s41598-025-97933-0
- Deng, H., Li, B., & Qin, X. (2022). Early versus delay oral feeding for patients after upper gastrointestinal surgery: a systematic review and meta-analysis of randomized controlled trials [Review of Early versus delay oral feeding for patients after upper gastrointestinal surgery: a systematic review and meta-analysis of randomized controlled trials]. Cancer Cell International, 22(1). BioMed Central. https://doi.org/10.1186/s12935-022-02586-y
- Dipasquale, V., Laganà, F., Arrigo, S., Trimarchi, G., Romeo, C., Navarra, G., Mattioli, G., Gandullia, P., & Romano, C. (2022). Enhanced Recovery Care versus Traditional Care after Surgery in Pediatric Patients with Inflammatory Bowel Disease: A Retrospective Case-Control Study. Biomedicines, 10(9), 2209. https://doi.org/10.3390/biomedicines10092209
- Dr Dinesh ROL 18 oct.pdf. (n.d.). Ellis, D., Agarwala, A. V., Cavallo, E., Linov, P., Hidrue, M. K., Carmen, M. G. del, & Sisodia, R. (2021). Implementing ERAS: how we achieved success within an anesthesia department. BMC Anesthesiology, 21(1). https://doi.org/10.1186/s12871-021-01260-6
- Elsayed, H. (2020). Enhanced recovery program after colorectal surgery. Al-Azhar International Medical Journal /Al-Azhar International Medical Journal, 0. https://doi.org/10.21608/aimj.2020.23737.1140
- Er, M., & ME, S. (2019). A Commonsense Patient-Centered Approach to Multimodal Analgesia Within Surgical Enhanced Recovery Protocols. DOAJ (DOAJ: Directory of Open Access Journals). https://doaj.org/article/7c8e13a9947943f4a2bc651c9b85b497
- Evans, D. C., Corkins, M. R., Malone, A., Miller, S. J., Mogensen, K. M., Guenter, P., & Jensen, G. L. (2020). The Use of Visceral Proteins as Nutrition Markers: An ASPEN Position Paper. Nutrition in Clinical Practice, 36(1), 22. https://doi.org/10.1002/ncp.10588
- Fakhar, N., Hyder, Z., Kasraianfard, A., Sharifi, A., Khamneh, A. C., Zarghami, S. Y., & Jafarian, A. (2021). Enhanced recovery after hepatopancreaticobiliary surgery: A single-center case control study. Annals of Hepato-Biliary-Pancreatic Surgery, 25(1), 97. https://doi.org/10.14701/ahbps.2021.25.1.97
- Fischer, C. P., Knapp, L., Cohen, M. E., Ko, C. Y., & Wick, E. C. (2021). Association of Enhanced Recovery Pathway Compliance With Patient Outcomes. JAMA Surgery, 156(10), 982. https://doi.org/10.1001/jamasurg.2021.2866
- Fu, G., Xu, L., Chen, H., & Lin, J. (2025). State-of-the-art anesthesia practices: a comprehensive review on optimizing patient safety and recovery [Review of State-of-the-art anesthesia practices: a comprehensive review on optimizing patient safety and recovery]. BMC Surgery, 25(1). BioMed Central. https://doi.org/10.1186/s12893-025-02763-6
- Gillis, C., Gill, M., Marlett, N., MacKean, G., GermAnn, K., Gilmour, L., Nelson, G., Wasylak, T., Nguyen, S., Araujo, E., Zelinsky, S., & Gramlich, L. (2017). Patients as partners in Enhanced Recovery After Surgery: A qualitative patient-led study. BMJ Open, 7(6). https://doi.org/10.1136/bmjopen-2017-017002
- Giménez‐Milà, M., Klein, A. A., & Martinez, G. (2016). Design and implementation of an enhanced recovery program in thoracic surgery. [Review of Design and implementation of an enhanced recovery program in thoracic surgery.]. PubMed, 8. National Institutes of Health. https://doi.org/10.3978/j.issn.2072-1439.2015.10.71
- Gramlich, L., Sheppard, C. E., Wasylak, T., Gilmour, L., Ljungqvist, O., Basualdo‐Hammond, C., & Nelson, G. (2017). Implementation of Enhanced Recovery After Surgery: a strategy to transform surgical care across a health system. Implementation Science, 12(1). https://doi.org/10.1186/s13012-017-0597-5
- Hao, T., Liu, Q., Lv, X., Qiu, J., Zhang, H., & Jiang, H. (2021). Efficacy and safety of early oral feeding in postoperative patients with upper gastrointestinal tumor: A systematic review and meta-analysis [Review of Efficacy and safety of early oral feeding in postoperative patients with upper gastrointestinal tumor: A systematic review and meta-analysis]. World Journal of Gastrointestinal Surgery, 13(7), 717. Baishideng Publishing Group. https://doi.org/10.4240/wjgs.v13.i7.717
- Heathcote, S., Duggan, K., Rosbrugh, J., Hill, B., Shaker, R., Hope, W. W., & Fillion, M. (2019). Enhanced Recovery after Surgery (ERAS) Protocols Expanded over Multiple Service Lines Improves Patient Care and Hospital Cost. The American Surgeon, 85(9), 1044. https://doi.org/10.1177/000313481908500951
- Huang, L. Y., Zhang, T., Wang, K., Chang, B., Fu, D., & Chen, X. (2024). Postoperative Multimodal Analgesia Strategy for Enhanced Recovery After Surgery in Elderly Colorectal Cancer Patients [Review of Postoperative Multimodal Analgesia Strategy for Enhanced Recovery After Surgery in Elderly Colorectal Cancer Patients]. Pain and Therapy, 13(4), 745. Adis, Springer Healthcare. https://doi.org/10.1007/s40122-024-00619-0
- Huh, Y., & Kim, D. J. (2021). Enhanced Recovery after Surgery in Bariatric Surgery [Review of Enhanced Recovery after Surgery in Bariatric Surgery]. Journal of Metabolic and Bariatric Surgery, 10(2), 47. https://doi.org/10.17476/jmbs.2021.10.2.47
- Jain, Y., Lanjewar, R., Lamture, Y., & Bawiskar, D. (2023). Evaluation of Different Approaches for Pain Management in Postoperative General Surgery Patients: A Comprehensive Review [Review of Evaluation of Different Approaches for Pain Management in Postoperative General Surgery Patients: A Comprehensive Review]. Cureus. Cureus, Inc. https://doi.org/10.7759/cureus.48573
- Jakobsson, J., Kálmán, S., Lindeberg-Lindvet, M., & Bartha, E. (2017). Is postspinal hypotension a sign of impaired cardiac performance in the elderly? An observational mechanistic study. British Journal of Anaesthesia, 119(6), 1178. https://doi.org/10.1093/bja/aex274
- Kaye, A., Urman, R., Rappaport, Y., Siddaiah, H., Cornett, E., Belani, K. G., Salinas, O., & Fox, C. (2019). Multimodal analgesia as an essential part of enhanced recovery protocols in the ambulatory settings [Review of Multimodal analgesia as an essential part of enhanced recovery protocols in the ambulatory settings]. Journal of Anaesthesiology Clinical Pharmacology, 35(5), 40. Medknow. https://doi.org/10.4103/joacp.joacp_51_18
- Li, W., Huang, S., Xie, Y., Chen, G.-Y., Yuan, J., & Yang, Y. (2022). Model-Based Computational Analysis on the Effectiveness of Enhanced Recovery after Surgery in the Operating Room with Nursing. Frontiers in Surgery, 9. https://doi.org/10.3389/fsurg.2022.922684
- Loria, C. M., Zborek, K., Millward, J. B., Anderson, M. P., Richardson, C. M., Namburi, N., Faiza, Z., Timsina, L., & Lee, L. S. (2022). Enhanced recovery after cardiac surgery protocol reduces perioperative opioid use. JTCVS Open, 12, 280. https://doi.org/10.1016/j.xjon.2022.08.008
- MacMahon, A., Rao, S. S., Chaudhry, Y. P., Hasan, S. A., Epstein, J. A., Hegde, V., Valaik, D., Oni, J. K., Sterling, R. S., & Khanuja, H. S. (2021). Preoperative Patient Optimization in Total Joint Arthroplasty—The Paradigm Shift from Preoperative Clearance: A Narrative Review [Review of Preoperative Patient Optimization in Total Joint Arthroplasty—The Paradigm Shift from Preoperative Clearance: A Narrative Review]. HSS Journal® The Musculoskeletal Journal of Hospital for Special Surgery, 18(3), 418. SAGE Publishing. https://doi.org/10.1177/15563316211030923
- Małczak, P. (2015). One Hundred Seventy-Nine Consecutive Bariatric Operations after Introduction of Protocol Inspired by the Principles of Enhanced Recovery after Surgery (ERAS®) in Bariatric Surgery. Medical Science Monitor, 21, 791. https://doi.org/10.12659/msm.893297
- Martín, D., Roulin, D., Grass, F., Addor, V., Ljungqvist, O., Demartines, N., & Hübner, M. (2017). A multicentre qualitative study assessing implementation of an Enhanced Recovery After Surgery program. Clinical Nutrition, 37(6), 2172. https://doi.org/10.1016/j.clnu.2017.10.017
- Modrzyk, A., Pasierbek, M., Korlacki, W., & Grabowski, A. (2020). Introducing enhanced recovery after surgery protocol in pediatric surgery. Advances in Clinical and Experimental Medicine, 29(8), 937. https://doi.org/10.17219/acem/121931
- Mohamed, Y., Hussein, A., Elsaba, O., Rhodes, M. J. C., Alloush, K., Elhofy, E., & Shokry, A. M. (2025). Optimizing Postoperative Outcomes in Abdominal Surgery: The Role of Enhanced Recovery After Surgery (ERAS) Protocols. Cureus. https://doi.org/10.7759/cureus.79258
- Othenin‐Girard, A., Ltaief, Z., Verdugo‐Marchese, M., Lavanchy, L., Vuadens, P., Nowacka, A., Gunga, Z., Melly, V., Abdurashidova, T., Botteau, C., Hennemann, M., Graf, J. D., Schoettker, P., Kirsch, M., & Rancati, V. (2025). Enhanced Recovery After Surgery (ERAS) Protocols in Cardiac Surgery: Impact on Opioid Consumption. Journal of Clinical Medicine, 14(5), 1768. https://doi.org/10.3390/jcm14051768
- Pache, B., Hübner, M., Martín, D., Addor, V., Ljungqvist, O., Demartines, N., & Grass, F. (2021). Requirements for a successful Enhanced Recovery After Surgery (ERAS) program: a multicenter international survey among ERAS nurses. European Surgery. Supplement/European Surgery, 53(5), 246. https://doi.org/10.1007/s10353-021-00698-9
- Park, J., Kim, E., Park, S., Han, W. K., Lee, J., Lee, J. H., & Nahm, F. S. (2023). Erector spinae plane block in laparoscopic colorectal surgery for reducing opioid requirement and facilitating early ambulation: a double-blind, randomized trial. Scientific Reports, 13(1). https://doi.org/10.1038/s41598-023-39265-5
- Park, S. H., Kang, S. H., Lee, S. J., Won, Y., Park, Y. S., Ahn, S.-H., Suh, Y., Park, D. J., & Kim, H. (2021). Actual compliance rate of Enhanced Recovery After Surgery protocol in laparoscopic distal gastrectomy. Daehan Nae’si’gyeong Bog’gang’gyeong Oe’gwa Haghoeji/Journal of Minimally Invasive Surgery, 24(4), 184. https://doi.org/10.7602/jmis.2021.24.4.184
- Pearsall, E., Meghji, Z., Pitzul, K., Aarts, M.-A., McKenzie, M., McLeod, R. S., & Okrainec, A. (2014). A Qualitative Study to Understand the Barriers and Enablers in Implementing an Enhanced Recovery After Surgery Program. Annals of Surgery, 261(1), 92. https://doi.org/10.1097/sla.0000000000000604
- Pędziwiatr, M., Kisialeuski, M., Wierdak, M., Stanek, M., Natkaniec, M., Matłok, M., Major, P., Małczak, P., & Budzyński, A. (2015). Early implementation of Enhanced Recovery After Surgery (ERAS®) protocol – Compliance improves outcomes: A prospective cohort study. International Journal of Surgery, 21, 75. https://doi.org/10.1016/j.ijsu.2015.06.087
- Pisarska, M., Gajewska, N., Małczak, P., Wysocki, M., Major, P., Milian-Ciesielska, K., Budzyński, A., & Pędziwiatr, M. (2018). Is It Possible to Maintain High Compliance with the Enhanced Recovery after Surgery (ERAS) Protocol?—A Cohort Study of 400 Consecutive Colorectal Cancer Patients. Journal of Clinical Medicine, 7(11), 412. https://doi.org/10.3390/jcm7110412
- Romero, A. D., Cuervo, B., Peláez, P., Miguel, L. de, Torres, M., Yeste, M., Alamo, M. M. R. del, Rubio, C. P., & Rubio, M. (2020). Changes in Acute Phase Proteins in Bitches after Laparoscopic, Midline, and Flank Ovariectomy Using the Same Method for Hemostasis. Animals, 10(12), 2223. https://doi.org/10.3390/ani10122223
- Roy, S., Kothari, N., Goyal, S., Sharma, A., Kumar, R., Kaloria, N., & Bhatia, P. (2022). Preoperative assessment of inferior vena cava collapsibility index by ultrasound is not a reliable predictor of post-spinal anesthesia hypotension. Brazilian Journal of Anesthesiology (English Edition), 73(4), 385. https://doi.org/10.1016/j.bjane.2022.04.001
- Seow‐En, I., Wu, J., Yang, L. W. Y., Tan, J. S. Q., Seah, A. W. H., Foo, F. J., Chang, M., Tang, C. L., & Tan, E. (2020). Results of a colorectal enhanced recovery after surgery (ERAS) programme and a qualitative analysis of healthcare workers’ perspectives. Asian Journal of Surgery, 44(1), 307. https://doi.org/10.1016/j.asjsur.2020.07.020
- Sier, M. A. T., Dekkers, S. L., Tweed, T. T. T., Bakens, M. J. A. M., Nel, J., Bastelaar, J. van, Greve, J. W. M., & Stoot, J. H. M. B. (2024). Morbidity after accelerated enhanced recovery protocol for colon cancer surgery. Scientific Reports, 14(1). https://doi.org/10.1038/s41598-024-67813-0
- Soteropulos, C. E., Tang, S. Y. Q., & Poore, S. O. (2019). Enhanced Recovery after Surgery in Breast Reconstruction: A Systematic Review [Review of Enhanced Recovery after Surgery in Breast Reconstruction: A Systematic Review]. Journal of Reconstructive Microsurgery, 35(9), 695. Thieme Medical Publishers (Germany). https://doi.org/10.1055/s-0039-1693699
- Starkweather, A., & Perry, M. (2017). Enhanced Recovery Programs and Pain Management. Topics in Pain Management, 32(8), 1. https://doi.org/10.1097/01.tpm.0000513202.87691.49
- Stethen, T. W., Ghazi, Y. A., Heidel, R. E., Daley, B. J., Barnes, L., Patterson, D., & McLoughlin, J. M. (2018). Walking to recovery: the effects of missed ambulation events on postsurgical recovery after bowel resection. Journal of Gastrointestinal Oncology, 9(5), 953. https://doi.org/10.21037/jgo.2017.11.05
- Stuart, C. M., Dyas, A. R., Mott, N. M., Bata, K., Bronsert, M. R., Kelleher, A. D., McCabe, K. O., Erickson, C., Randhawa, S., David, E. A., Mitchell, J. D., & Meguid, R. A. (2024). Postoperative day of surgery ambulation improves outcomes following lung resection: a multicenter prospective cohort study. Journal of Thoracic Disease, 16(11), 7300. https://doi.org/10.21037/jtd-24-1183
- Taniguchi, H., Sasaki, T., & Fujita, H. (2012). Preoperative Management of Surgical Patients by “Shortened Fasting Time”: A Study on the Amount of Total Body Water by Multi-Frequency Impedance Method. International Journal of Medical Sciences, 9(7), 567. https://doi.org/10.7150/ijms.4616
- Teeuwen, P. H. E., Bleichrodt, R. P., Strik, C., Groenewoud, J. J. M., Brinkert, W., Laarhoven, C. J. H. M. van, Goor, H. van, & Bremers, A. J. A. (2009). Enhanced Recovery After Surgery (ERAS) Versus Conventional Postoperative Care in Colorectal Surgery. Journal of Gastrointestinal Surgery, 14(1), 88. https://doi.org/10.1007/s11605-009-1037-x
- Thompson, C., French, D., & Costache, I. (2018). Pain management within an enhanced recovery program after thoracic surgery [Review of Pain management within an enhanced recovery program after thoracic surgery]. Journal of Thoracic Disease, 10. AME Publishing Company. https://doi.org/10.21037/jtd.2018.09.112
- Trotta, M., Ferrari, C., D’Alessandro, G., Sarra, G., Piscitelli, G., & Marinari, G. M. (2019). Enhanced recovery after bariatric surgery (ERABS) in a high-volume bariatric center. Surgery for Obesity and Related Diseases, 15(10), 1785. https://doi.org/10.1016/j.soard.2019.06.038
- Tweed, T. T. T., Sier, M. A. T., Daher, I., Bakens, M. J. A. M., Nel, J., Bouvy, N. D., Bastelaar, J. van, & Stoot, J. H. M. B. (2022). Accelerated 23-h enhanced recovery protocol for colon surgery: the CHASE-study. Scientific Reports, 12(1). https://doi.org/10.1038/s41598-022-25022-7
- Wells, S. J., Austin, M. T., Gottumukkala, V., Kruse, B., Mayon, L., Kapoor, R., Lewis, V. O., Kelly, D., Penny, A., Braveman, B., Shkedy, E., Crowder, R., Moody, K., & Swartz, M. C. (2021). Development of an Enhanced Recovery Program in Pediatric, Adolescent, and Young Adult Surgical Oncology Patients. Children, 8(12), 1154. https://doi.org/10.3390/children8121154
- Wobith, M., & Weimann, A. (2021). Oral Nutritional Supplements and Enteral Nutrition in Patients with Gastrointestinal Surgery [Review of Oral Nutritional Supplements and Enteral Nutrition in Patients with Gastrointestinal Surgery]. Nutrients, 13(8), 2655. Multidisciplinary Digital Publishing Institute. https://doi.org/10.3390/nu13082655
- Yoon, S., & Lee, H. (2024). Challenging issues of implementing enhanced recovery after surgery programs in South Korea. Anesthesia and Pain Medicine, 19(1), 24. https://doi.org/10.17085/apm.23096
- Zhang, J., Che, J., Sun, X., & Ren, W. (2022). Clinical Application of Perioperative Anaesthesia Management Based on Enhanced Recovery after Surgery Concept to Elderly Patients Undergoing Total Knee Replacement. Computational Intelligence and Neuroscience, 2022, 1. https://doi.org/10.1155/2022/8039358
- Zhang, Y., Liu, Z., Ma, L., Li, X., Zhu, Q., Wang, G., Cang, J., Diao, Y., Zhang, T., Shen, L., & Huang, Y. (2025). Current state and future education implication of enhanced recovery after surgery (ERAS) among Chinese anesthesiologists: national repeated cross-sectional surveys from 2019 to 2023. BMC Medical Education, 25(1). https://doi.org/10.1186/s12909-025-07351-z
- Zhou, B., Ji, H., Liu, Y., Chen, Z., Zhang, N., Cao, X., & Meng, H. (2021). ERAS reduces postoperative hospital stay and complications after bariatric surgery. Medicine, 100(47). https://doi.org/10.1097/md.0000000000027831
- Zorrilla‐Vaca, A., Stone, A. B., Ripollés‐Melchor, J., Abad‐Motos, A., Rodríguez, J. M. ́Ramírez, Galán-Menéndez, P., Mena, G. E., Grant, M. C., García-Pérez, C., Higuera-Míguelez, E., Vidal, J. M. M., Merino-García, M., Rubio-López, A., Pascual-Diez, M. E., García-Miguel, F. J., Cabezudo-Sanjose, L. R., Martínez-Díaz, R., Alegría-Rebollo, S., González-Rodríguez, J. L., … Arias-Romano, A. (2021). Institutional factors associated with adherence to enhanced recovery protocols for colorectal surgery: Secondary analysis of a multicenter study. Journal of Clinical Anesthesia, 74, 110378. https://doi.org/10.1016/j.jclinane.2021.110378