Administering fluids to children during surgery isn’t just about hydration—it’s a delicate balancing act that requires precision. Kids aren’t just small adults; their bodies respond differently to fluid imbalances, making proper assessment and prescription crucial.
Why Fluid Management in Children Matters
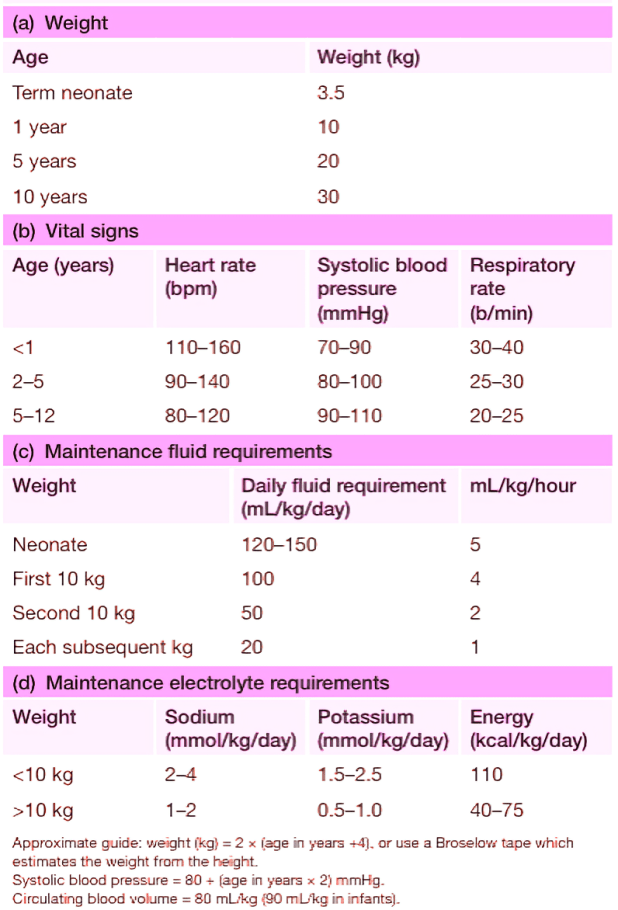
Before giving any fluid or medications, healthcare providers must consider:
- The child’s weight
- Vital signs (heart rate, blood pressure, capillary refill)
- Fluid and electrolyte needs compared to normal ranges
Dehydration can be tricky to spot in children. Key signs include:
- Moderate dehydration (5% fluid loss):
- Dry mouth
- Sunken eyes and fontanelle (in infants)
- Reduced urine output
- Severe dehydration (>10% fluid loss):
- Poor skin elasticity (tenting)
- Lethargy or drowsiness
- Rapid heart rate (tachycardia)
- Weak pulse and delayed capillary refill (>2 seconds)
The Hidden Danger: Hyponatraemia in Kids
Children are more vulnerable to hyponatraemia (low sodium levels) than adults because their brains take up more space in the skull. Severe cases can lead to:
- Seizures
- Permanent brain damage
- Even death
Common causes of hyponatraemia in surgical settings:
- Using hypotonic fluids (like 0.18% saline) for resuscitation instead of balanced solutions.
- Giving excessive fluids (3–5 times more than needed).
UK guidelines recommend maintenance fluids with sodium levels between 131–154 mmol/L to prevent complications.
Key Learning Objectives
✔ Understand the four main reasons for IV fluids in children
✔ Calculate fluid rates based on weight (see reference tables)
✔ Recognize the risks of low-sodium fluid
✔ Know how illness and surgery affect fluid balance
✔ Identify and manage hyponatraemia (<135 mmol/L)
Tonicity & Osmolarity of Fluids: What You Need to Know
Not all IV fluids are created equal. Some terms to remember:
- Isotonic fluid (like 0.9% saline) match blood’s electrolyte balance.
- Hypotonic fluid (like 0.18% saline + glucose) can dilute sodium levels dangerously.
When and How to Prescribe Fluids
Fluids are given for four main reasons:
1. Emergency Resuscitation (Shock or Severe Dehydration)
- Fluids used: 0.9% saline, blood, or 4.5% albumin (colloid)
- Dosage: 10–20 mL/kg over 10–20 minutes (repeat up to 40 mL/kg if needed)
2. Replacing Lost Fluids (Pre-existing Deficits)
- Fluids used: 0.9% saline + potassium (KCl) or Hartmann’s solution
- Given over 24–48 hours with regular monitoring
3. Ongoing Losses (Bleeding, Vomiting, Drainage)
- Replace losses mL-for-mL (e.g., 4.5% albumin for protein loss)
4. Maintenance Fluids (Post-Surgery or Fasting)
- Avoid hypotonic fluids (0.18% saline is unsafe outside neonates)
- Reduce to 70% of usual rate for 24 hours post-surgery (stress makes the body retain water)
🚨 Warning: Don’t increase fluid just because urine output drops—this can worsen hyponatraemia!
Managing Hyponatraemia: Act Fast!
- Mild (Na >125 mmol/L, no symptoms): Fluid restriction
- Severe (Na <125 mmol/L with seizures/lethargy):
- 3% hypertonic saline (1 mL/kg over 15 min)
- Transfer to PICU immediately
Special Considerations for Neonates
- First 48 hours: 10% glucose at 60 mL/kg/day
- Day 2 onward: Add sodium (0.18%) and potassium (0.15%)
- Preterm/low birth weight babies: May need up to 180 mL/kg/day
🔍 Monitor glucose! Keep levels above 2.6 mmol/L to prevent complications.
Final Takeaway of paediatric fluids managements:
Fluid management in children requires careful calculation, monitoring, and quick action when imbalances occur. By following evidence-based guidelines, we can keep young patients safe before, during, and after surgery.
Need a quick reference? Bookmark this guide for easy access to pediatric fluid best practices!
Read more paediatric surgery topics: Paediatric surgery
Guidelines & Research
- NICE Guidelines on IV Fluids in Children – Official UK recommendations for pediatric fluid management.
- WHO Dehydration Treatment Guidelines – Global standards for managing dehydration in children.
- American Academy of Pediatrics (AAP) on Hyponatremia – Expert insights on preventing and treating low sodium levels.